In college, when many of her friends were off celebrating the weekend at a football game or a party, Theresa Dinh, ’15, could often be found on the periphery.
As a trained EMT with University of Richmond Emergency Medical Services (UREMS), she stood at the ready, equipped with a radio and a medical bag, waiting for the call that someone on campus needed her attention.
“I remember being in Spanish class one time and getting a call,” she said. “Everyone heard the phone ring, and they stopped to let me see what the situation was. And then I was out the door, responding to the emergency.
“When I came back, class was over, but some of them stayed to watch over my stuff and catch me up on what I missed. It never felt like a burden. Everyone was understanding and it gave me the confidence that I could do this job.”
Dinh signed up for UREMS in hopes of gaining hands-on experience in the field she aspired to enter and, like many of her colleagues, found it to be a crucial stepping stone. Dinh is one of eight graduates from the Class of 2015 who are now working as physicians, surgeons, ER doctors, anesthesiologists, and medical researchers. Their time with UREMS both affirmed their plans to pursue medicine and led them to find their place within an expansive field.
“I had real patient care responsibilities, which is unusual at the undergraduate level,” said Nick Rothbard, ’15. “Being able to speak to those experiences and how they shaped me as a person when applying to medical school — it was undoubtedly very helpful.”
ANSWERING THE CALL
UREMS is a student-run organization with real-life situations and consequences. Members are trained and certified as Emergency Medical Technicians in Virginia, and they report to the Richmond Ambulance Authority. They’re often the first on the scene during a campus emergency, responding alongside the UR Police 24 hours a day, seven days a week.
“Even though we have the city’s EMS team, it’s important for us to be on campus,” Dinh said. “[Campus is] on the outskirts of town, so it might take RAA longer to respond. As the first on the scene, we could stabilize a patient or help a student having a medical emergency. Having us arrive first is helpful because we can make sure everyone is calm and safe.”
The organization functions much like any other emergency medical provider. When a call comes into the campus emergency number, it’s dispatched to two on-call students. They quickly arrive at the scene, either on foot or in a dedicated service vehicle, and provide immediate medical care until an ambulance arrives. A supervisor listens in and offers backup as needed. A chief of operations keeps the whole team organized, managing a schedule that ensures 24/7 coverage and appropriate on-site staffing at large campus events.
Despite the professional training and structure, students are learning on the job, and those first calls can be nerve-wracking.


“It’s so different applying that book knowledge to a real person and situation. ... The more shifts I did, the more comfortable I became with the routine and the things I needed to do.”
“As a pre-med student, I was good at reading, good at taking tests,” said Erica Yamamoto, ’15. “My EMS training was more or less the same. Then all of a sudden, I’m getting a call to go to D-hall because someone fell. It felt like everything I knew went out the window.
“It’s so different applying that book knowledge to a real person and situation; it was almost paralyzing. I don’t know if any class or test prepared me for that, but the more shifts I did, the more comfortable I became with the routine and the things I needed to do.”
By the time students graduate, they’ve learned to think on their feet and make decisions with confidence and speed. They’ve learned to balance the responsibilities of life with their on-call commitments. They know how to work together as a team. On ride-alongs with the RAA, they’ve witnessed more complex trauma cases and the challenges of responding to emergencies across the city of Richmond.
And for those who decide to apply to medical school, they have a strong sense of purpose and a clear-eyed understanding of the life they’re signing up for.
“[Admissions committees] want to know that you understand medical school is hard, that it’s a long process, and that you are resilient,” Dinh said. “UREMS gave me stories and experience to point to as proof that I had vetted this plan of mine.”
THE SURGEON: THERESA DINH, MD
After a few gap years working at a nonprofit healthcare organization serving the uninsured in Memphis, Dinh got a master’s in pharmacology and attended medical school at the University of Tennessee Health Science Center. She’s currently in her third year of general surgery residency at the University of Tennessee Health Science Center.
Given my EMS experience, I thought emergency medicine would be the next logical step, but during my rotations in medical school, I realized it wasn’t quite what I was looking for.
The case that did it for me was during my surgery rotation. It was a man who had skin cancer but was too old to go under general anesthesia, so we had to operate while he was awake. They called me up, handed me a scalpel and a knife, and I excised the cancer and bandaged him up. All I could think was, “We just cured this guy of cancer.”

Surgery is very hands-on, and it’s instant gratification. You see the problem, decide how to fix it, and then you do it. It’s like when I was an EMT, and I could help someone and see the outcome pretty quickly. People would call us on their worst days, and I was able to help alleviate their pain and suffering. It’s very humbling.
I’m in my third year of residency now, and there’s quite a bit of overlap [between emergency medicine and surgery]. We have the largest Level 1 trauma center in town, so we get all of the trauma cases. I saw the pre-hospital care with UREMS and, now that I’m on the hospital side, I understand what the scene might have looked like before a patient got to us. It’s a natural segue from EMS to hospital emergencies.
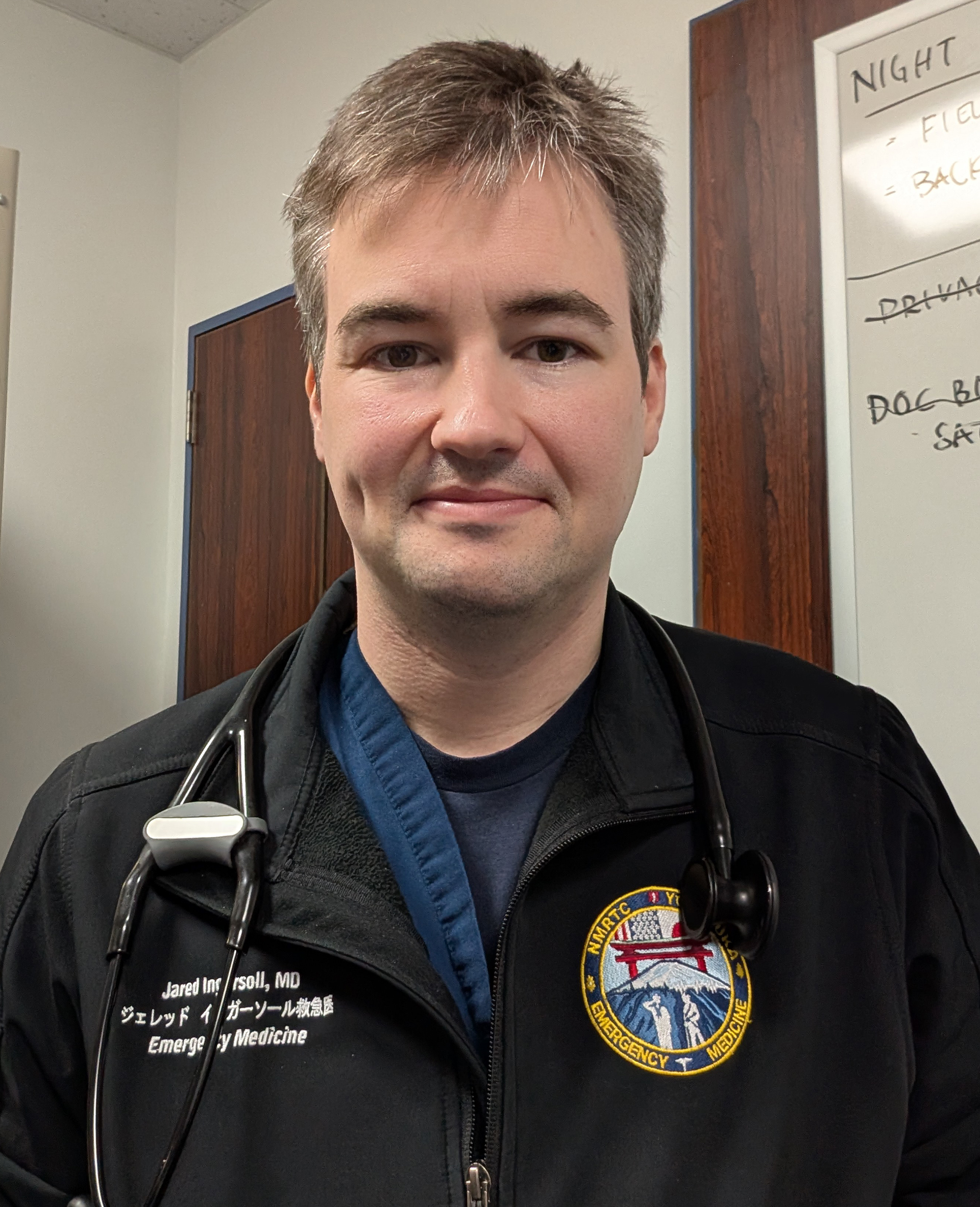
THE MILITARY ER DOCTOR: JARED INGERSOLL, MD
Ingersoll spent a year working for RAA before joining the Navy and enrolling in medical school at Uniformed Services University in Bethesda, Maryland. He completed his residency at the Naval Medical Center in San Diego and is currently stationed in Japan, where he works as an emergency medicine physician.
“It’s definitely unpredictable, and I like that. I don’t get anxious. It’s like a brand-new slate every day.”
My senior year, a group of us went to a conference for collegiate EMS organizations. I went to a lecture by a retired Army surgeon who detailed his time serving overseas in Iraq and Afghanistan. That’s when I got the idea of doing military medicine. I didn’t know it was an option.
One of the big draws of military medicine is that it’s similar to emergency medicine. You have to do the best you can with what you have. I thought that was an interesting and challenging angle. It makes decisions more complicated.
I work at a small naval hospital that sees active-duty military, their spouses and children, as well as retirees and a few civilian contractors working and living around the base. I’m one of five ER doctors. I’m also the EMS director for the naval bases on mainland Japan. It felt like a full circle when I was told I’d be overseeing part of the pre-hospital care.
Emergency medicine feels like a rewarding use of my time because I can focus on trying to diagnose and rule out life-threatening and urgent conditions. Then I send patients where they need to go. It’s definitely unpredictable, and I like that. I don’t get anxious. It’s like a brand-new slate every day.
THE FAMILY DOCTOR: ERICA YAMAMOTO, DO
After graduating, Yamamoto took a gap year and returned home to New Jersey, where she worked as a medical scribe. She attended medical school at Des Moines University in Des Moines, Iowa, and a rural family medicine residency in Monroe, Wisconsin. She then completed an integrative medicine fellowship at the University of Madison. She now works at Ohio State University.
“Being an EMT was the start of helping me find myself within medicine, and I am grateful for the experience. ”
My current position involves doing osteopathic manipulative therapy and integrative medicine consults, which is very different from my time as an EMT.
When volunteering as an EMT, it is easy to assume that you could advance your career by going into emergency medicine or working in critical care because those are the teams that you work closely with. However, when I was applying to medical school, I was still unsure of what I wanted to do. I ended up shadowing all kinds of specialties, like a radiologist, a plastic surgeon, and family practice. Once I was in medical school and started rotations, I enjoyed working with all population groups and learning a little bit of everything, which is why I ultimately went into family medicine.
For my residency, I matched into my top choice in a rural family medicine clinic in Monroe, Wisconsin. It was during the peak of the COVID-19 pandemic, and the culture of medicine changed a lot during that time. I saw the loss of trust in the medical system and found that my patients would ask me about alternatives that I was not equipped to discuss. This motivated me to pursue an integrative medicine fellowship so that I could learn about things outside of the traditional Western medical model.
When I reflect on my undergraduate experience, it is now easier to see how being an EMT was not quite right for my personality, but participating in UREMS taught me so much about what it means to be in the medical field. Having first-hand experience in caring for others, especially when patients were not doing well or were not kind, forced me to evaluate if I could see myself working with people who are suffering.
Being an EMT was the start of helping me find myself within medicine, and I am grateful for the experience.
THE ANESTHESIOLOGIST: NICK ROTHBARD, DO
Rothbard attended the Touro College of Osteopathic Medicine and completed his anesthesiology residency at the University of Minnesota. He is currently pursuing a one-year cardiothoracic anesthesiology fellowship at the University of Minnesota.

“UREMS was also my first introduction to how working in medicine affects small decisions in your daily life.”
The hands-on nature of EMS appealed to me, but ultimately, emergency medicine wasn’t the right fit for my personality. But critical care medicine and cardiac anesthesiology are also very hands-on. I do intubations every day. I place central lines and arterial lines. I manage cardiovascular physiology. I respond to cardiac arrests in the operating room. UREMS introduced me to that acute care environment.
Cardiovascular physiology is interesting in the context of heart surgery, where the physiology of the heart is altered by anesthetics, the cardiopulmonary bypass machine, and the surgery itself. It takes a lot of quick thinking and decision-making, and a deep understanding of cardiovascular physiology to make good decisions for a patient whose heart is sometimes functioning very poorly. You build close relationships and a lot of trust with the cardiac surgeons to help some really sick and complicated patients through complex surgeries.
UREMS was also my first introduction to how working in medicine affects small decisions in your daily life. As a cardiac anesthesia fellow, I do home call, which means that I’m at home with a pager and at any moment, I could be paged to come into the hospital for a surgical emergency. You have to structure your life around that. If I had a test, I would have to communicate with other members of UREMS to hold the radio and backpack for those two hours. There’s a natural give-and-take of working with a close team that’s important in medicine.